Reflections: Past And Present

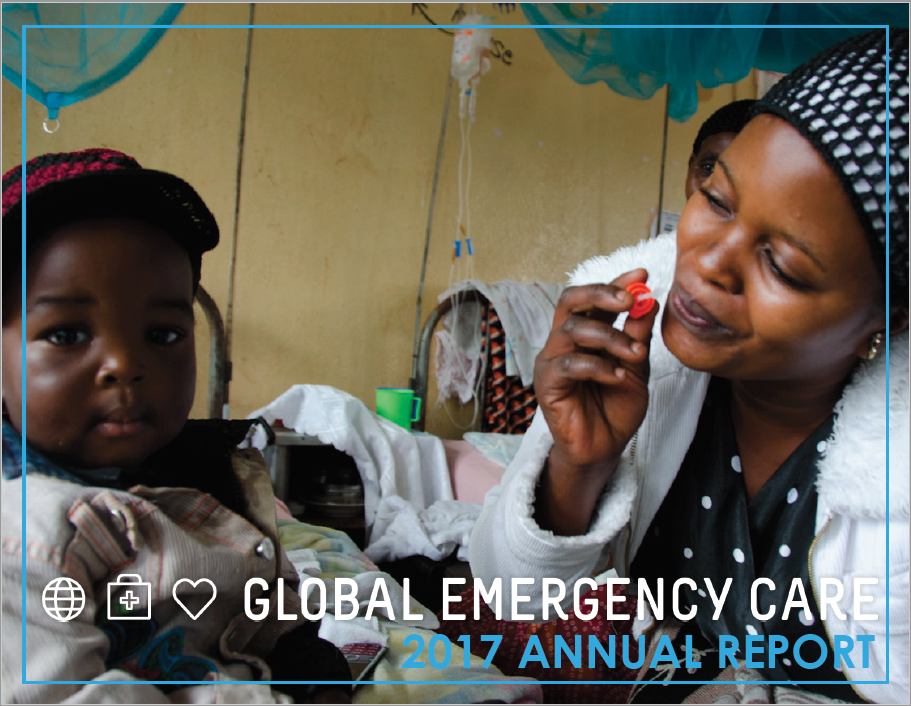
This week, I watched as Jovita, a qualified ECP, evaluated a patient brought in with a recent miscarriage. The woman had lower abdominal pain for one day. Jovita examined her and immediately realized she had an infection. She performed an ultrasound that confirmed her suspicion – retained products from the pregnancy were slowly becoming infected. Jovita started antibiotics immediately and the patient had the products removed the following morning before the infection damaged her internal organs or spread throughout her system. This young woman left the hospital and was doing well on follow up.
Back in 2006, I remember seeing a patient on the ward who had arrived the night before with an open fracture (i.e. the bone was sticking out) of his lower leg. This injury has a very high risk for infection and the longer one delays washing it out and giving antibiotics, the higher the risk of infection. In the 12 hours he had been at the hospital, he had a dry gauze dressing placed over the wound and was given a dose of Tylenol. He received no emergency care.
On the second night of my recent visit, I walked into the ED to find Hilary, our Education Director and newly qualified ECP, applying a splint. When I asked what happened to the young woman, he said – “open fracture, Doctor. We washed it out under pethidine [strong pain medication], closed the wound, and gave antibiotics. I am just splinting her so she can recover from the ward.” The patient appeared to have adequate pain control as Hilary applied the splint. I looked around and saw that Hilary provided quality care for the patient with other hospital staff without any physician interaction. I’m proud to see the growth of Nyakibale’s ECPs providing life saving care to a very needy population, and to see the significant impacts GECC’s emergency care training program is having on the health outcomes of the local patient population.
– Dr. Mark Bisanzo, President and Co-Founder, GECC


This Post Has 0 Comments