
The Hard Bargain To Save Lives

Dr. Prisca
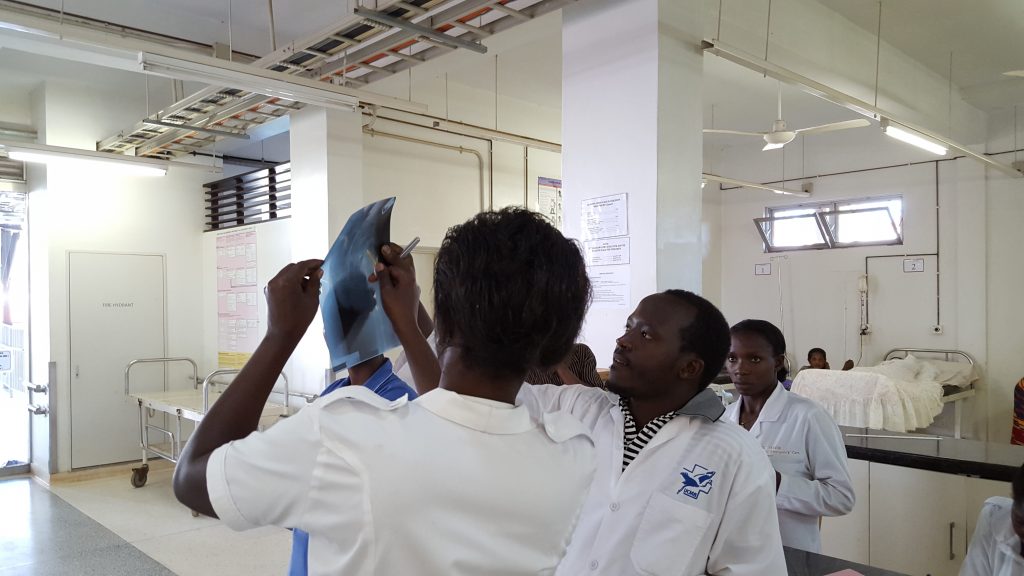
Dr. Prisca Kizito is a GEC-sponsored EM physician and an assistant lecturer at Mbarara University of Science and Technology (MUST) in the emergency medicine department. In addition to training the diploma students, her role is to teach primarily post-graduate students and stretches to undergraduate students in their surgical rotation. Mostly done are bedside teaching and handling handover rounds, which are the essential bits of understanding and critical thinking in inpatient care. “Those rounds help us bring the diploma and post-graduate students together to think and work collaboratively as they are supervised. It allows for the discussion of important and intriguing cases so that we can enhance the learning process,” she says.
Her training in EM was one arduous journey. Like any new venture, paving the way for a new profession in a country where EM is barely visible was a daunting task. “Being the pioneer class, we were literally the guinea pigs for the master of EM course. We had to be prepared, opened minded, persistent, and goal-oriented to learn in terms of academics and to grow as a person,” she says. It was not easy for them because of limited resources. Theirs was a class of five students with four or five modules per semester, one full-time lecturer supported by a visiting lecturer, and limited teaching materials. “We learned to live within our means and to improvise with what was available, which was challenging. I grew emotionally and became self-aware,” she says. They had to build and foster relationships with lecturers from the traditional departments to have their modules delivered to progress in the course.
Undertaking the course stretched her, pushing her beyond every kind of comfort that she had known. “This is a full-time course away from home. I had to hand over my initial responsibilities like work, leave family and friends behind, and everything that was familiar to me to move to a new region in Uganda to undertake the course. It was a tough decision to move,” she recalls. It was also a choice between earning an income and studying. For her, it meant no source of income, no parties, and the like to focus on work, work, and more work. “It was so tiring… The three years weren’t easy, but we are so glad it is all done,” she says with a big sigh of relief.
But the struggle is not yet over. “Our biggest need is academic resources and training equipment to enable repetitive action for effective learning and the gaining of competencies. We need more academic faculty to reduce the burden on the current team so that as lecturers, we can provide better support to our students,” she says. Prisca is also advocating for scholarships for EM professionals. She says, “This will motivate more professionals who would be in EM but are currently held back by limited finances.” There is also a need to formally structure EM professionals at all levels to create demand for EM professionals.
“EM has been the most engaging and interesting journey in my career,” she says, having joined the profession in 2017. She recalls a case of a 15-year-old child who came in with severe bradycardia (slowed-heart beat) of 18 beats per minute. She was on duty, and they searched for the underlying cause using every possible means, but nothing worked. They managed with their usual procedures (atropine and adrenaline), but every time they would stop the drugs, the boy would fall back and get reduced blood flow to the rest of his body. “I remember staying overnight, watching to see how the child could be helped because I knew that this condition could be reversed at the Uganda Heart Institute in Kampala, some 269.5kms away. We found an ambulance and put the boy on adrenaline for the whole journey of 5 hours. For the risk and benefit analysis… well, we just wanted the boy alive so that he could get the specialist care that he needed,” she says. About two days later, she received information that the child had survived, received treatment, and was alive! “This experience was all a bargain for me because I could have easily given up given the obstacles. But then, I knew that this child could die if nothing was done. And yet he could live if someone could just do the right thing to put the heartbeat back to the right rate,” she beams with an infectious smile.
In Uganda, the call for life or death is usually a bargain because of inadequate emergency care. You can help us increase the chances of survival among vulnerable communities by donating to this cause. Click HERE to donate and feel free to tell someone about the cause!
Keeping Tabs on GEC Work in South-Western Uganda

John Bosco Kamugisha
John Bosco Kamugisha is the Programme Coordinator for GEC in Uganda. Currently,
GEC is in collaboration with Mbarara University of Science and Technology (MUST) in south-western Uganda to train emergency care practitioners (ECPs) in Uganda. His human resource role involves coordinating trainers and all the activities for the program as well as providing curriculum oversight for the course.
JB, as he is popularly known by colleagues, was first introduced to emergency care when he met the president of GEC back in 2006 – 2007 while working at Nyakibale Hospital in Rukungiru district. “At that time, there was no emergency care in the hospital. It is so unfortunate that people would die because there was no one to offer the specialized care needed for emergencies,” he recollects.
Then, things began to unfold. In 2007, the Emergency Department was started in the hospital, and in 2008, training for hospital staff on job commenced. But it was not sustainable because although it offered skills, it didn’t have professional accreditation. “Later, when we had understood what was needed and streamlined our processes, we started providing certificate and diploma courses,” he says.
In 2015, the team engaged Masaka Regional Hospital to pilot the project that was in Rukungiri. And in 2017, MUST approved the advanced diploma program that enabled them to offer accredited programs. Since then, Uganda has graduated two cohorts, with the third expected next year. And to scale up the course, a new curriculum is under review by the relevant academic authorities in Uganda to upgrade the advanced diploma program to a bachelor’s degree in emergency medicine.
One of the gaps hindering the development of ECPs is the limited space at Masaka Hospital and Mbarara Hospital, which cannot accommodate more than ten students at a time. “If we can have more space, then we can admit more students,” JB says.
On the bright side, the Ministry of Health in Uganda has supported the team with scholarships for students. This is a clear indication of the government’s recognition of the need to develop emergency medicine in the country. Uganda now has a master’s program in EM offered at MUST and Makerere University, with MUST having graduated its first class, while Makerere University is set to graduate its first class this year. Emergency Medicine is a new specialist profession; people are beginning to see the fruits, and some universities are beginning to consider it.
The role of EPCs was highlighted at the time of COVID-19, especially in the Masaka region, one of the hotspots in Uganda. Some of the ECPs were deployed as frontline workers at the Uganda-Tanzania border to man the Covid-19 testing center, while others were deployed at the Covid-19 unit in Masaka Hospital. “Covid-19 was pretty engaging for us. With the skills acquired in emergency care, I remember working on a family that included a mother, father, and child who had contracted Covid-19. We provided the best kind of care they needed. All the affected members survived, and they are alive, happy, and living productive lives,” JB says.
Looking into the future, JB is very hopeful. He says, “We have seen considerable progress from where we started to where we are now. We want to scale up our training to support everyone involved in emergency care.”
GEC has made significant strides since 2017, starting with diplomas to now having EM accredited at higher levels of training. This is a significant achievement in providing lifesaving care for vulnerable communities in Uganda, and we invite you to support this cause. You can do so by donating to help us train emergency care professionals to save lives. Click HERE to donate and remember to tell a friend to tell a friend!
Welcoming New Team Members!

GEC is thrilled to welcome Steven Kisingiri to our team as the inaugural Country Director in Uganda. He comes with 23 years of experience in International Development, and is interested in collaborative and creative approaches to build community and reach vulnerable populations.
He is excited to be a part of a dynamic and caring team, dedicated to saving lives. Steven is dedicated to creating opportunities for ordinary people to realize their potential no matter the circumstances they face. This goal has stayed at the core of his work. In his words, “The thrill for me has always been creating a fighting chance for people, and seeing people blossom as a result is priceless.”
Steven is the father to three amazing girls, and in his spare time enjoys gardening, golf, and spending time with friends and family.

Q&A with Steven Kisingiri, Country Director in Uganda
What excites you about GEC and why did you decide to join the organisation?
I have always had a fascination with Emergency Departments from when I was much younger. I even dreamt of setting up one! I have to embarrassingly admit that the 1994-2009’s TV drama ER had something to do with it. So, I have learned throughout my career how important human life is.
How do you see this transferring to your work at GEC?
In my past career I have done this by giving the poor and most vulnerable in society a hand-up – as opposed to handouts – and these came in the form of educational opportunities for those who could not afford, life skills, food, shelter, and so on. Being part of the GEC team, on the other hand, provides an opportunity to develop a cadre of health care professionals who provide high-quality care that ultimately reduces the number of people who die, needlessly suffer from a disease or medical condition, or even become disabled. This really does excite me about this new chapter in my career…it is like a dream come true!
What are you most looking forward to doing during your tenure?
I am passionate about seeing a collaboration with the Ministry of Health, academic institutions, and like-minded partners in training and developing thousands of emergency professionals whose key goal is to ensure no life is limited due to an easily treatable illness or injury at any health center and hospital. Not only will these professionals be skilled at what they do, but they will also have the capacity to develop the next generation of emergency care workforce in the region and the rest of Africa! The work ahead of us is not going to be easy. But I am part of a great GEC team that is up to the challenge and committed for the long haul.
Working Through Adversity on the Frontlines
This past year has exposed health disparities around the world. Uganda is no exception.

At the beginning of the year, Covid-19 levels were low, but Uganda and other African countries were expected to see exponential contagious spread. The first cases of Covid-19 in Uganda were sent to one of Global Emergency Care’s partner hospitals in Masaka, Uganda, putting our Emergency Care Practitioners (ECPs) on the front lines as the pandemic spread across sub-Saharan Africa. Our ECPs, stationed in rural hospitals in the Rukungiri, Masaka, and Mbarara Districts, are the communities’ best hope for triaging Covid-19 symptoms and providing research-based public health education to a population already plagued with misinformation and fear.
Kansiime Glorious, like many of our ECPs, has taken on extra responsibility in orienting the hospital staff about the proper use of PPE, hand hygiene, and triaging COVID-19 patients. In her words, “The country’s economy has suffered as many businesses, schools, and others that involve gatherings are still under lockdown.” The economic crises in Uganda due to Covid-19 led to high transport fees and resource shortage. As Covid-19 surged in Uganda, our ECPs were recognized by the Ugandan Ministry of Health as the first front-line workers to begin the treatment and management of Covid-19. Over 200 Covid-19 patients were treated by ECPs at the Masaka hospital and the Tanzania border crossing.
Updates From the Field
Learning from a difficult year and looking towards the future

Despite the challenges brought on by Covid-19 and election-related restrictions by the government, GEC was able to continue the trajectory of our work in Uganda.
Especially as the world works to emerge from the pandemic, GEC is so grateful for funding from our incredible partners and donors that make this work possible. With limited funding opportunities from Grantmakers as they reduced their budgets during 2020, support from donors like you enabled GEC-trained Emergency Care Practitioners to be deployed to hospitals, including 3 hospitals where new Emergency Departments have been founded.
We are also excited to announce that with generous support from donors, the first cohort of Masters of Emergency Medicine students graduated from Mbarara University.

Our partner hospitals have predicted that the PPE supplies for our ECPs working on the front lines of the pandemic response will last through April. As the vaccination rate slowly increases and current COVID levels remain manageable, we are working to maintain accessible emergency care and transition management of the ECP training and education fully to our local partners. Your support continues to make this possible.
We are working very closely with the 5 of them to take over a more supervisory role of the ECP cadre. Additionally, a GEC-trained MMed graduate was appointed as the president of the Emergency Care Society of Uganda.
Building a more sustainable future together
Dear GEC family,
Today, I’m writing with some very exciting news about the future direction of GEC. As many of you know, it has been a long-term goal of the organization to transition our leadership structure from one where the executive team consists mainly of north Americans to a more Ugandan-led, sustainable leadership team with a focus on co-creation. In that spirit, it is with great enthusiasm that I welcome the newest addition to the GEC family – Mr. Steven Kisingiri – GEC’s pioneer Uganda Country Director. Steven was recently hired after a highly competitive hiring process. In this new position, Steven will lead efforts to strengthen GEC’s strategic partnerships, while growing the ECP program and working to fully integrate it into the medical and educational systems in Uganda. We are all very excited to have an individual of Steven’s caliber as our inaugural Country Director, and we look forward to his leadership.
In conjunction with Steven’s hire, I am stepping down as Executive Director. I’d like to express my appreciation to the entire GEC extended family for giving me this opportunity. Although I will be stepping down from the ED role, I will continue to work with the GEC team as an advisor, and am grateful for the continued involvement. While it is bittersweet for me personally, I am very proud of what we’ve accomplished together, and I’m enthusiastic for what the future holds for the ECP cadre and for emergency care development across Uganda.
To that end, I would like to give a warm GEC welcome to our new Executive Director – Dr. Ashley Pickering. Ashley has been working with GEC for many years and has extensive experience working with the GEC team in Uganda, as well as supporting GEC’s work from the U.S. Ashley’s role as the new Executive Director will be focused on facilitating the growth and expansion of organizational leadership to Steven and our Ugandan colleagues. We are all very enthusiastic about Ashley’s new leadership, and look forward to working with her to advance GEC’s mission and vision.
I’m very proud that with these changes we are actively transitioning GEC leadership to a more sustainable and Ugandan-led organizational structure, in accordance with our long-term vision. I look forward to collaborating with the entire team for a successful transition as we continue to train new ECPs, provide high quality emergency care, and help build an accessible emergency care system for all Ugandans.
Thank you to each and every one of you for your continued support.
Warmest regards,
Tom Neill
Emergency Care in Low Resource Settings
By: Birungi Alfunsi

“The beauty of being in the emergency department is the feeling you get when you save a life. The little one who is brought in with hypoglycemia will shortly smile at you when it has been corrected. The mother will be smiling, and tears will be dry. Most interesting is when you help someone breathe.”
I am Birungi Alfunsi, an Emergency Care Practitioner, with 10 years of practice experience in the rural emergency care setting in Uganda.
Here I discuss the critical aspects of the practice of emergency care in low resource setting. Little is known about the availability and utilization of emergency care services in developing countries, here referred to as low resource settings.
When the need for emergency care arises, there are only two options: a) appropriate intervention to save a life, or b) no intervention and lose a life.
The beauty of being in the emergency department is the feeling you get when you save a life. The little one who is brought in with hypoglycemia will shortly smile at you when it has been corrected. The mother will be smiling, and tears will be dry. Most interesting is when you help someone breathe.

Normally in low resource settings, the interventions to emergencies are largely provided by general practitioners with no appropriate training in delivering emergency care services. Most of the time those emergencies are managed as other conditions, as they would be on a normal outpatient day without consideration of the golden hour (the only time left for intervention or to lose a life).
In some areas, an emergency is only understood as a trauma and treatment rooms are labeled as causality wards. The rest of the non-trauma cases are treated in the outpatient department.
More resources in education and training are required to score higher in emergency care in low resource settings. Equipment such as glucometers, pulse oximeters, defibrillators, and many others are not available for use due to the lack of trained staff, not so much due to the cost as one might expect.
All in all, emergency care in low resource settings remains a big arena to pay attention to, where education and skills development can have an outsized impact for saving lives.

We’re Hiring a Country Director!

Many of you know that part of our long term vision for Global Emergency Care has been to transition the leadership structure to a more sustainable, Ugandan-driven, and Ugandan-owned leadership structure with a focus on co-creation. The time has come to take steps toward fulfilling that vision.
That’s why today I am very excited to announce that GEC will begin the process to hire a new Country Director (CD) to be based in Uganda. The Country Director will have strategic and operational responsibility for Global Emergency Care’s staff, programs, and execution of its mission, while reporting to the Board of Directors.
COUNTRY DIRECTOR JOB DESCRIPTION
How to Apply
This position is now closed.
Applications will be accepted until 11:59pm on 10 February 2021 East Africa Time.
We look forward to collaborating with the Ugandan team for a successful transition as we continue to train new ECPs, provide high quality emergency care, and help build an accessible emergency care system for all Ugandans.
The Role of Sample Collection and Management during the Covid-19 pandemic

By: John Bosco Kamugisha, Msc, Emergency Care Practitioner, Masaka Program Coordinator
My role during the pandemic was sample collection and management for Masaka Hospital’s Coronavirus Response Team. This includes collection, packing, refrigeration, recording, and transporting samples.
In the beginning people feared to take samples, so I boldly accepted to be trained to do sample management. My two colleagues and I trained other regions on how to do sample management which helped to increase human resource capabilities, and reduce the staffing gaps in management of Covid-19. Being on the frontline as a sample manager, I used to pick follow up samples from the Covid-19 Treatment Unit which was a tough task in the beginning because no one wanted to be exposed. In the middle we faced a lot of stigma arising from colleagues who didn’t want us to be close to them.
The worst stigma was when I went to the market to buy food and the vendor said “you work in corona so I can’t touch your money” It affected me so much but later I improved. Even our colleagues used to call us Covid-19 and this increased stigma outside work place.
My role as a sample management officer is key in that I can collect appropriate sample and send it in time for early diagnosis then I follow up on contacts if one person turns positive. Contact tracing helps to reduce the transmission of the virus. Sample management is also key in that if results are positive or negative it helps to isolate those who are suspected to have the virus.
Life has changed since the President started to uplift the lock down. Many shops are open, markets stores, schools, and other institutions. People used to follow the guidelines but as time went on and no one was dying most Ugandans are no longer following guidelines.
Many people no longer put on masks, any soap or sanitizer at the work place. Many people believe that Covid-19 is a ‘hoax” and is being politicized. The campaigns for elections have made things worse because no one is now following any guidelines. We anticipate that there might be an influx of cases after elections.
Let’s stay safe, sanitize, wash our hands, wear masks correctly, and protect our families.
Working as an ECP during COVID-19

By: Kansiime Glorious
Kansiime Glorious is an Emergency Care Provider working in a low-resource setting, hospital in Masaka, Uganda who is very passionate about her work.
How was your role critical in Uganda’s coronavirus response?
Being an Emergency Care Provider has taught me to attend to the pandemic as a community emergency. I started by orienting the fellow hospital staff about the proper use of personal protective equipment, hand hygiene, and the proper triaging of patients at the hospital gate, emergency department, and the outpatient department. Due to our capability shown in daily patient care, I was transferred, along with other ECPs, to the Covid-19 treatment unit by the hospital director as they expected very sick Covid-19 patients.

How has your role as an ECP changed since the pandemic began?
As the pandemic has gone viral in the community, very sick patients present to the emergency department. By applying the knowledge and skills of approaching very sick patients, we have improved patient care because not every patient with Covid-19-like symptoms has specifically Covid-19, and there is a likelihood of other respiratory infections.
How have things changed as the pandemic has evolved and the country has opened back up?
Being a regional referral hospital, the government provides personal protective equipment. Intensive care facilities are being put in place with equipment needed as the backup and continuous emphasis on maintaining standard operating procedures in daily work by the health sector. The country’s economy has suffered as many businesses, schools, and others that involve gatherings are still under lockdown.
Working as an Emergency Care Practitioner

By: Teddy Kiire
“Big ideas come from forward thinking people and challenge the norm, think outside the box and invent the world they see inside than submitting to the limitations of current dilemmas”. – T.D Jakes
Teddy Kiire is my name. I’ve been working as an Emergency Care Practitioner for the past 10 years with Global Emergency Care, and that’s where my story started.
Years ago, I had no idea what it would feel like to be an ECP, but here I am to share with you what it feels like. It’s now my passion and I am very happy, and at the same time satisfied with my career choice. I encourage people to undertake emergency medicine because it comes with personal satisfaction of knowing one’s work directly to engage with patients.
WHY IS EMERGENCY MEDICINE A GREAT CAREER TO ME AS AN ECP
As an ECP, I initiate care for patients with urgent, higher acuity illness, traumas, and injuries to provide acute resuscitation and stabilization of patients with life threatening emergencies. To love this career, one must understand how to recognize and quickly manage complex patient needs. For the time I have practiced as an ECP, I have mastered the skills of multi-tasking, prioritization, and working with a care team.
The main summary reason That I love being an ECP is that it is both challenging and personally rewarding. You directly and quickly see the benefits and positive results of your diagnosis and treatment of patients with emergent conditions. You will have that satisfaction of knowing you have a big positive differences in patients’ lives and wellbeing. This aspect is what makes emergency medicine so interesting and stimulating.
Throughout my practice, Emergency medicine encompasses a nice mix of diagnostic medicine and performing diagnostic and therapeutic procedures like bedside ultrasound, incision and drainage, paracentesis etc.
CHALLENGES
The fact that emergency medicine is quite a new course here in Uganda is a challenge. There is still a lot to be done, but we can’t stop being positive.
So, I personally love the challenges that come with adopting to the ECP roles. Today’s challenge, as an ECP, is to be able to work in a very stressful environment with high volume of patients and limited resources.
It’s amazing how the ECP role has advanced since 2008. I am grateful for the advocacy that Global Emergency Care has provided nationally within different states to clarify our roles and scope of practice, while not forgetting my fellow ECPs because ours is not a one day dream.
To sum it all, emergency medicine is a great career that the national health care system should adopt to it. We shall not stop until we get there, “The struggle continues”!
To support Teddy, the ECPs, and the struggle, please consider a donation to GEC today:
Ultrasound in Resource-Limited Settings: A Case Based, Open Access Text
Faculty at UC Davis Health in collaboration with the California Digital Library (CDL) and Blaisdell Medical Library are pleased to announce the release of Ultrasound in Resource-Limited Settings: A Case Based, Open Access Text. This new online resource aims to provide an open access clinical resource for radiologists and clinicians who practice ultrasound in low and limited resourced healthcare settings. The project was conceived of and developed by two UC Davis Health physicians: Michael Schick and Rebecca Stein-Wexler, with help from Aida Nasirishargh as the online editor. Drs. Schick and Stein-Wexler have been teaching and using ultrasound for many years in some of the least resourced healthcare settings in the world. In these regions, most people have no access to diagnostic imaging. Ultrasound is particularly positioned to help fill this gap as the most portable, inexpensive, and versatile form of diagnostic imaging.
“While caring for patients and teaching ultrasound in the most low resourced health settings in the world, we routinely diagnose illnesses such as rheumatic heart disease and extra-pulmonary tuberculosis,” said Dr. Schick. “Many conditions we encounter are considered ‘neglected’ and rare in high income countries, but are becoming increasingly relevant with global travel, migration, and population displacement. When we tried to learn more about the ultrasound diagnostics of these diseases and find high quality images and videos for teaching our global trainees, we noticed a lack of available resources. Standard texts offer ample education about diseases that are common throughout the world. However, they fall short in building the expertise that is needed by those who practice in limited-resourced and tropical regions.”
The team’s goal was to create an up-to-date and useful resource for those who use ultrasound to take care of vulnerable patients around the globe. Drs. Schick and Stein-Wexler envisioned a text that was concise and clinically relevant, with high quality images and discussion that could be easily accessed, shared and downloaded in areas with limited internet bandwidth — a living text that would be translated into multiple languages and continue to grow as future impactful cases were identified and new techniques were discovered.
The project is a collaborative effort by health care practitioners worldwide who use point-of-care and comprehensive ultrasound. Each chapter is authored by experts with case-based knowledge of both ultrasound and the highlighted disease. The chapters are 100% case based and provide important insight into how experts practice medicine and apply ultrasound in the limited resourced healthcare setting. As you scroll through chapters, high quality videos (in bandwidth-efficient GIF format) play automatically, and full-resolution video files are available for download and sharing.
When Drs. Schick and Stein-Wexler consulted with Blaisdell Medical Library about publishing options for this unique work, health sciences librarian Amy Studer saw the opportunity to connect them with CDL to investigate the possibility of hosting their work on an open access publishing platform. “This publication, by virtue of its intended audience and goals, is particularly concerned with issues of accessibility and discoverability, and CDL’s eScholarship Publishing program shares that commitment. We regard this publication as an important step forward in redesigning medical publications for the specific needs of users in the field,” says Studer.
Because of the large number of videos and images needed to illustrate the concepts in the text, CDL identified the Manifold platform as the best system for building and displaying the work. “Foundational to the Manifold platform is the ability to harness dynamic web content as an integral component of a publication, layering text and media alongside one another in an intuitive reader that encourages thoughtful engagement,” said Terence Smyre, Manifold Digital Projects Editor. “Manifold’s open-source, open-access ethos is also specifically aimed at the public good — values that align strongly with the goals of the project.”
This publication also represents the first project completed under the eScholarship Labs program at California Digital Library. “We launched the Scholarship Labs program in 2019 with the aim of fostering innovation in scholarly publishing by piloting new publishing technologies to support experimental forms of scholarship,” said Justin Gonder, Senior Product Manager, Publishing at CDL. “Manifold has now graduated from the Labs program and is available for use by any member of the University of California community who has a scholarly project in mind that requires deep integration of text and media.” For more information, visit the eScholarship Help Center.
In the coming months, Ultrasound in Resource-Limited Settings will be released in several different languages including Spanish and Farci, initially, with many others to follow. If you would like to contribute to additional translations of this resource, please contact the editors: mschick@ucdavis.edu and rsteinwexler@ucdavis.edu.
Ultrasound in Resource-Limited Settings: A Case Based, Open Access Text is available now at:
https://manifold.escholarship.org/projects/ultrasound-in-resource-limited-settings
Michael Schick DO, MA, DIMPH, FACEP
Associate Clinical Professor, Emergency Medicine
Director, International Ultrasound
Co-Director, Technology Enabled Active Learning
Director of Ultrasound, Global Emergency Care
Rebecca Stein-Wexler, M.D.
Professor of Radiology
Section Chief, Pediatric Radiology
Director, Global Radiology Education and Outreach
University of California, Davis Medical Center
and UC Davis Children’s Hospital















